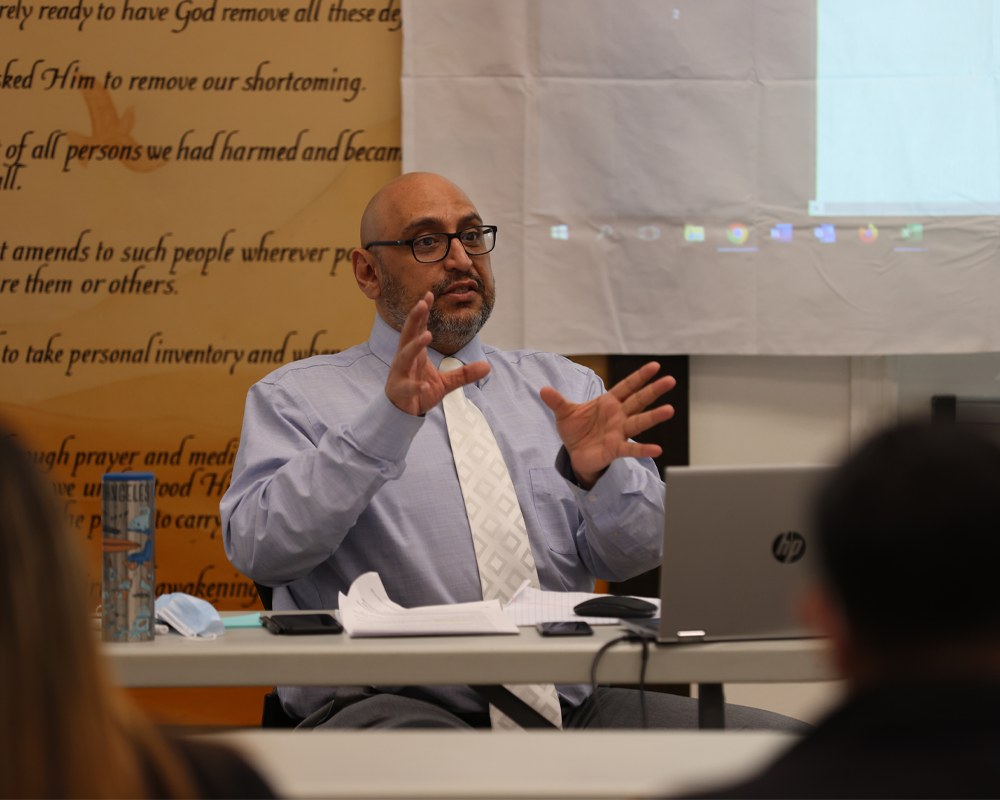
On February 17, Social Model Recovery Systems conducted an “Admission Process and Documentation Training” led by our Senior Clinical Director, Pedram Moshfegh.
The training focused on the New SMRS Admission and Real Time Quality Control Review Process, ASAM Assessments, Treatment Planning, and Discharge Planning. A thorough review of proper documentation including patient’s medical history, current health status, diagnosis, treatment plan, and any other relevant information related to the patient’s care was also included. This documentation is typically maintained in a patient’s medical record, which is a legal document that provides a comprehensive history of the patient’s health and treatment.
The new admission and real-time quality control review process for alcohol and drug treatment program involves several steps to assess the patient’s needs and create an individualized treatment plan. Accurate and complete documentation is crucial for ensuring the safety and quality of patient care. It provides healthcare providers with important information to guide clinical decision-making, track a patient’s progress over time, and ensure continuity of care between different healthcare providers.
Documentation typically includes the patient’s demographic information, medical history, physical exam findings, diagnostic test results, medication orders, treatment plans, and progress notes. The type and level of detail included in documentation will depend on the healthcare setting and the specific needs of the patient.
It is important to note that patient documentation is subject to legal and regulatory requirements, including patient privacy laws such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States which was also discussed in the training. Healthcare providers are responsible for maintaining accurate and confidential patient records and should follow established policies and procedures to ensure the security of patient information.

Ms. Nancy Crosby, Mental Health Clinical Program Head of SAPC (Los Angeles County Substance Abuse and Prevention Control) also gave training via zoom on Inter-County Transfer of Medi-Cal recipients. According to Ms. Crosby, this is the first time SAPC had ever conducted an individualized agency training about the Inter-County Transfer process. Inter-County Transfer of Medi-Cal refers to the process of transferring a Medi-Cal case from one county to another. Medi-Cal is the California version of the Medicaid program, which is a health insurance program for low-income individuals and families. When a person applies for Medi-Cal benefits, they are generally enrolled in the county in which they reside. However, if a person moves to a different county, they may need to transfer their Medi-Cal benefits to the new county.

Overall, the new admission and real time quality control review process for alcohol and drug treatment programs are designed to provide a comprehensive evaluation of the patient’s needs and to create a personalized treatment plan that can help them achieve their recovery goals. This training served to enhance the staff’s ability to take the necessary steps to ensure all clients are receiving the best individualized treatment on their journey of recovery.
Call 877-50-SOCIAL or 877-507-6242 for confidential support & treatment options if you or someone you know needs help.




